Melanoma: Prevention and Early Detection
Skin cancer is the most common form of cancer in the United States.1 Melanoma, a type of skin cancer, is particularly dangerous. Although it accounts for only 1% of skin cancer cases, melanoma spreads quickly to lymph nodes, is less curable than other skin cancer types, and is responsible for most skin cancer deaths.2
This article will discuss prevention and early detection of melanoma. It will also explain a simple method that patients can use to screen themselves, and how the lab can help patients with melanoma.
Scope of the Problem
The American Cancer Society (ACS) estimates that in 2020 about 100,000 new cases of melanoma will be diagnosed, and about 7,000 people will die from melanoma.2 The incidence of melanoma has been steadily increasing for the past 30 years and is expected to continue to increase.3 The average age at diagnosis is 65 years, but melanoma is not uncommon in people as young as 30 years.2
Risk Factors
Melanoma is one of the most preventable forms of cancer. Sun exposure, especially if sunburn occurs, is the leading risk factor, as is exposure to sources of artificial ultraviolet (UV) light such as tanning beds. Based on their individual characteristics, some people are more at risk than others (see Sidebar).3-5
Prevention
In 2014 the Surgeon General issued a Call to Action report to address the increasing burden of melanoma. The report identifies groups of people who would most benefit from increased disease education and awareness that reducing exposure to UV radiation can prevent most skin cancers.6 Since the Call to Action was released, melanoma awareness and prevention have increased, but a comprehensive national program for skin cancer prevention is yet to be implemented in the United States.
A number of measures can help prevent melanoma. Counseling in primary care settings has been proven to modify behavior and decrease intentional tanning.6 The United States Preventive Services Task Force (USPSTF) recommends that clinicians counsel patients with fair skin who are 10 to 24 years old to minimize their exposure to sunlight and artificial UV light to decrease their risk of developing melanoma.3 The ACS recommends several precautions for people (see Sidebar) at increased risk of getting melanoma5,7:
- Avoid prolonged exposure to midday sun
- Wear a wide-brimmed hat
- Wear tightly woven clothing that covers arms and legs
- Wear sunglasses that block both UVA and UVB rays
- Use a broad spectrum sunscreen with an SPF of 30 or higher
- Avoid indoor tanning
Fortunately, melanoma is highly curable when detected in its early stages. The 5-year relative survival rate is 99% if caught early, at the localized stage, but only 25% for individuals with distant metastasis.8 However new treatments, such as immunotherapy, have revolutionized the treatment of advanced melanoma. A study has indicated that some regimens can result in 5-year survival rates of 50% or more for select people with advanced melanoma.9
Early Detection
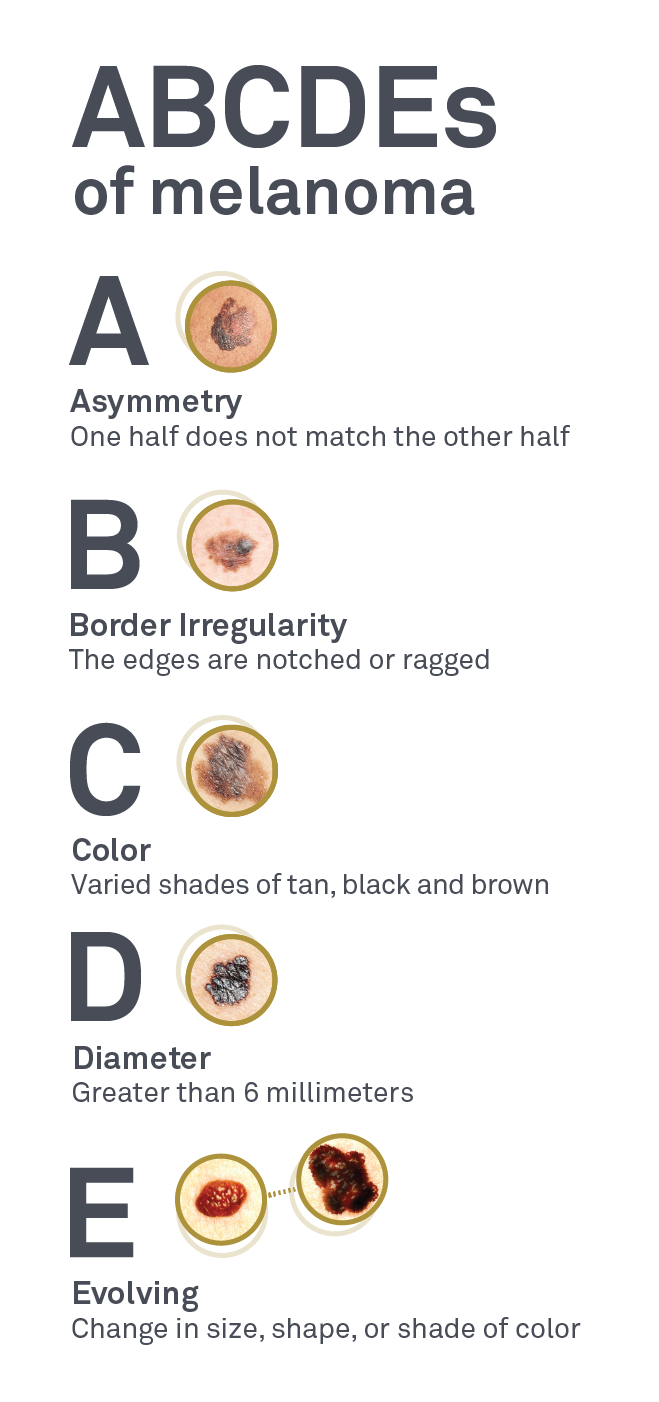
Visual screening during a total body skin examination (TBSE) is an easy and effective way to detect new or changing moles. Given the lack of available evidence, the USPSTF does not currently support annual TBSE by a clinician.5 However, for at-risk patients (see Sidebar), many organizations and clinicians disagree.3 Regardless of this controversy, patients are encouraged to examine themselves each month using the ABCDE rule to identify suspicious moles (Figure).10,11
Figure. What to Look for in a Mole: The ABCDEs10,11
(Image Source: Dermpath Diagnostics)
Risk Factors for Melanoma3,5
- Aged 35 to 75 years
- Personal history of skin cancer
- Family history of skin cancer
- Light skin
- Blond or red hair
- More than 40 moles
- 2 or more atypical moles
- Many freckles
- Sun-damaged skin
- History of blistering sunburn
- History of indoor tanning
How the Laboratory Can Help
Dermpath Diagnostics, a Quest Diagnostics company, offers a comprehensive test menu for dermatological needs, including testing of skin biopsies with analysis performed by board-certified dermatopathologists. In addition to tests for heredity and tumor burden, Dermpath offers BRAF/c-KIT testing for patients with metastatic melanoma. Dermpath and Quest also offer companion diagnostic tests including PD-L1 IHC 288 pharmDx test, used to detect PD-L1 expression in melanoma tissue; Melanoma, BRAF V600 Mutation, Cobas®; and Melanoma, BRAF V600E and V600K Mutation Analysis, THxID™. Together with microsatellite instability testing, these tests help identify candidates for targeted immune therapy.4
Note: Dermpath and Quest contract independently with insurance companies.
References
- Skin cancer (including melanoma)—patient version. National Cancer Institute. Accessed March 24, 2020. https://www.cancer.gov/types/skin
- Key statistics for melanoma skin cancer. American Cancer Society. Updated January 8, 2020. Accessed March 24, 2020. https://www.cancer.org/cancer/melanoma-skin-cancer/about/key-statistics.html
- Johnson MM, Leachman SA, Aspinwall LG, et al. Skin cancer screening: recommendations for data-driven screening guidelines and a review of the US Preventive Services Task Force controversy. Melanoma Manag. 2017;4:13-37.
- Leonardi GC, Falzone L, Salemi R, et al. Cutaneous melanoma: from pathogenesis to therapy (Review). Int J Oncol. 2018;52:1071-1080.
- Risk factors for melanoma skin cancer. American Cancer Society. Revised August 14, 2019. Accessed March 24, 2020. https://www.cancer.org/cancer/melanoma-skin-cancer/causes-risks-prevention/risk-factors.html
- Skin cancer prevention progress report. Centers for Disease Control and Prevention. Reviewed August 15, 2019. Accessed March 24, 2020. https://www.cdc.gov/cancer/skin/what_cdc_is_doing/progress_report.htm
- How do I protect myself from UV rays? American Cancer Society. Updated July 23, 2019. Accessed March 24, 2020. https://www.cancer.org/cancer/skin-cancer/prevention-and-early-detection/uv-protection.html
- Survival rates for melanoma skin cancer. American Cancer Society. Revised January 8, 2020. Accessed March 24, 2020. https://www.cancer.org/cancer/melanoma-skin-cancer/detection-diagnosis-staging/survival-rates-for-melanoma-skin-cancer-by-stage.html
- Larkin J, Chiarion-Seleni V, Gonzalez R, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2019;381:1535-1546.
- Detect skin cancer. American Academy of Dermatology. Accessed March 24, 2020. https://www.aad.org/public/spot-skin-cancer/learn-about-skin-cancer/detect
- What to look for: the ABCDEs of melanoma. American Academy of Dermatology. Accessed March 24, 2020. https://www.aad.org/public/diseases/skin-cancer/find/at-risk/abcdes
Content reviewed 5/2020